Patient Eligibility and Replacement Schedules
Article ID: 1623
Eligibility
When speaking with patients about when they are eligible for items, it is important to make sure we are not leaving them with misconceptions about what eligible means. Being eligible for an item means...
-
the patient's insurance provider will approve the item in question be sent out to the patient
-
they will cover a percentage of the item as outlined in the patient's policy (so long as there is no deductible that the patient has yet to meet)
When requesting supplies for a patient, we should NOT leave them with the perception that their supplies will be free. A good rule to follow is that we should not try to speak to any specifics when it comes to a patient's insurance because we do not have any details. Here are some phrases that we should avoid using (and why):
If it shows you are eligible, your insurance will cover it…
This is incorrect for two reasons:
-
Our system may not be up to date, or there may be a pending supply request from the HME
-
Patients may have a deductible that they have to meet, which means they would be responsible for the full cost of the items until their deductible is met. Alternatively, a patient may have a co-pay they will be required to cover depending on their insurance provider.
We will only send the items you are currently eligible for….
This statement is fine to use, so long as you clarify that they are responsible for any co-pay or unmet deductible.
Your local branch will contact you before shipping your supplies if you have any out-of-pocket expenses…
Since we do not know the billing practices for our HMEs, we should not be telling patient that they will be contacted because we can not be sure (unless otherwise stated in Salesforce). If the patient insists on knowing their out-of-pocket expenses for a supply request, we can offer to send a request to have the HME contact them.
CAUTION: If we do send a request to have the HME contact the patient, we should not promise that this will happen. Instead, advise the patient that we will ask the HME to contact them prior to shipping out their supplies.
Replacement Schedules
During your calls, patients may ask about how many supplies they will be receiving in their supply requests or how frequently a patient needs to change their supplies. These questions can be difficult to answer, as we can't be certain how many of each item a patient will receive because these amounts are dictated by their insurance provider. If asked, we can provide patients with suggested replacement schedules, but we should avoid telling patients that they will be receiving enough supplies to follow this schedule. This is especially true for patients who have Medicaid or Medicare for their insurance providers. Please see the table below for the suggested replacement timeframes.
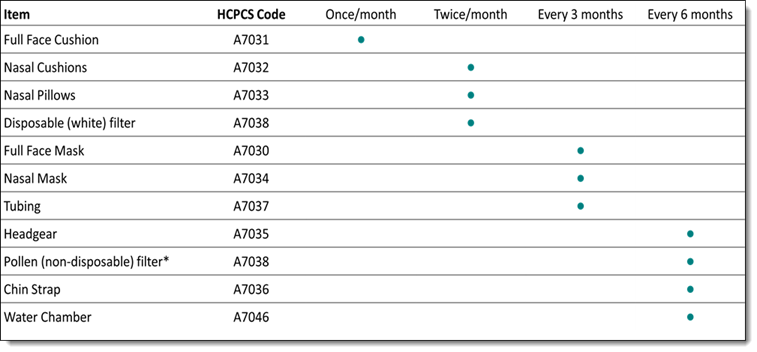
If a patient asks why they did not receive enough supplies to meet these suggested timeframes, explain to them that different insurance providers may not follow this schedule firmly and that they (the timeframes) are suggestions, not rules.
CAUTION: If we do send a request to have the HME contact the patient, we should not promise that this will happen. Instead, advise the patient that we will ask the HME to contact them prior to shipping out their supplies.
- Article Metadata
- The following table provides management and control details about the current published version of this article.
Prepared By
Clint Rodenfels
Reviewed By
Clint Rodenfels
Process Owner
Diane Clarke
Subject Matter Expert
Nader Omar
Visibility
Internal - ACE
Revision Workflow
Standard
Archive Date
DAC
DAC1
- Revision History
- The following table summarizes changes for each published version of this article.
Date
Changes
29 February 2024
Add tags: supply times, replacement schedule. Update format to current standard (remove tabled structure). Add drop shadow to the image. Minor revisions for clarity. (K00289)
3 June 2019
Initial publication. All new content.
